- Global shipping from each location
Female Fertility and Testing

We didn’t know that becoming pregnant was not as easy as getting sperm into a turkey baster and voila you are pregnant. After speaking to others, most don’t know this either. We learned that you only have a short window to get pregnant in your monthly cycle. On top of that, many factors contribute to how fertile you are and how difficult it will be to get pregnant. Things like, do you still ovulate? What are your FSH levels? What about progesterone and estrogen? Add your AMH ( how many eggs you have left) and form what seems to be a complicated process.
Those who know us and have followed our story will see that we got our fertility tested and our results left us with a lot to be desired which is why we were encouraged to conceive simultaneously—leading us to fall pregnant 12 days apart on our 1st and 2nd cycle.
First, visit your doctor and get them to run some tests to check your fertility. These blood tests are done on day 2/3 of your cycle, which means 2/3 days after you start bleeding (not spotting).
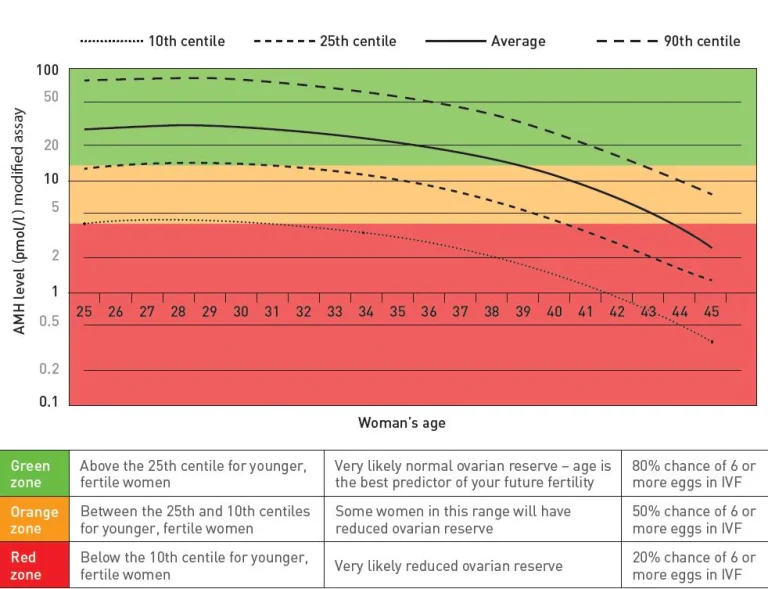
AMH (Anti-Mullerian Hormone) indicates your ovarian reserve, i.e. what your egg stores are.
FSH (Follicle-stimulating hormone) is responsible for stimulating the growth and maturation of your egg.
Oestradiol is a hormone triggered by FSH and they work together to develop the egg follicle further.
Progesterone helps control the amount of FSH released by the pituitary gland. It is also responsible for creating the environment where the egg implants into the uterus. We call this the sticky hormone.
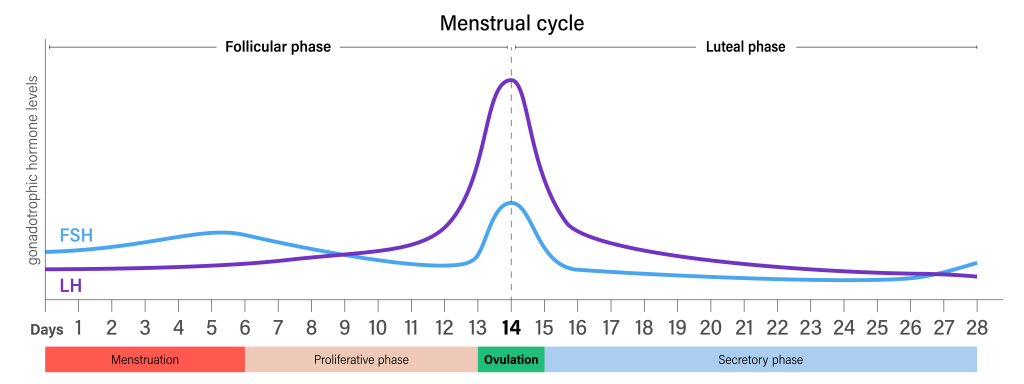
LH (luteinizing hormone) plays different roles in the two halves of the menstrual cycle. In weeks one to two of the cycle, LH is required to stimulate the ovarian follicles in the ovary to produce oestradiol. Then, around day 14 of the cycle, a surge in LH causes the ovarian follicle to tear and release an egg from the ovary.
Our doctor ordered other tests to check general health with the knowledge that we wanted to conceive. These included: Complete blood count, Diabetic profile, Thyroid function test, Rubella antibodies, STD, Hepatitis B, Hepatitis C, C-reactive protein, Liver function test, Iron, Hepatitis C, HIV, Serum B12, and folate.
The AMH is your anti-müllerian hormone, which tells you the level of eggs left in your body (your egg reserve). Unfortunately, if this is low, there is nothing that you can do about it. My partner Kat and I had low AMH levels for our age; however, we could still conceive. Low does not mean any. A high result may indicate that you have PCOS; however, this will be detected in conjunction with other hormones.
See the below graph on AMH levels vs your age
Follicle Stimulating Hormone (FSH) There are different views on what would be classified as the “normal” range; however, most reports indicate that anything above 15 is considered “abnormal.” On average, women in the 10-to-15 range have a 50% lower success rate of falling pregnant than others in their age group with FSH levels of 9.5 or below.
If FSH levels are abnormally high, the body needs to work harder to produce more FSH to stimulate egg maturation and ovulation. This could indicate a less-than-ideal quality and quantity of eggs in the ovaries. This is a normal part of aging and is more common in women aged 38 or older. However, even young women can have high FSH levels. So if you have a high FSH, don’t worry. This doesn’t mean you can’t have a baby; you may have more difficulty and potentially need IVF treatment. The FSH test is used in conjunction with other tests that look at LH, estradiol, and progesterone levels to determine a person’s ovarian reserve.
FSH levels can also be abnormally low. This is usually combined with low LH levels and may indicate a problem with the functioning of the pituitary gland or hypothalamus, which are two parts of the brain that play an essential role in ovulation. Anything lower than 3 is considered low.
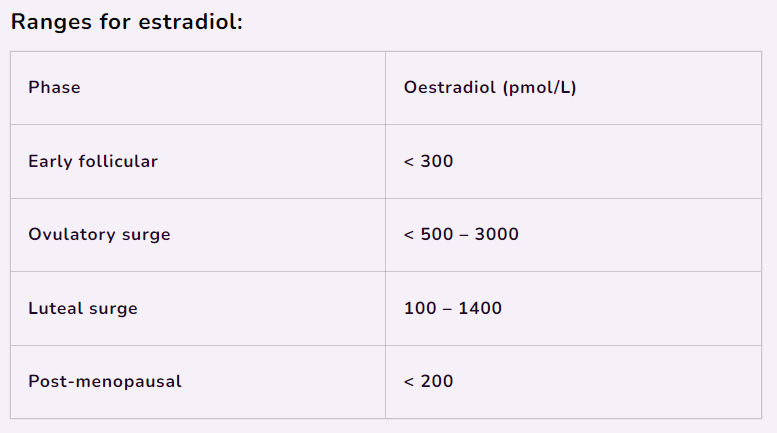
High estradiol levels indicate that you might have a problem with your ovarian reserve. It could also mean that the estradiol is suppressing FSH. Either of these things could mean that you will have more trouble getting pregnant, more trouble ovulating (even with treatment), and reduced success with IVF.
If your estradiol levels are low, it can indicate polycystic ovary syndrome (PCOS) or hypopituitarism.
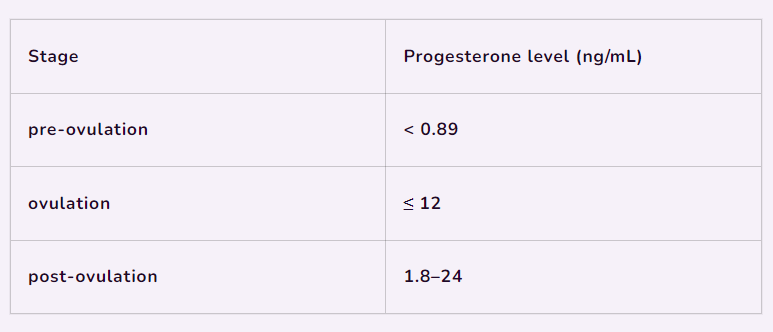
High levels of progesterone typically don’t cause any adverse health effects. Having high levels of progesterone won’t cause any negative impact on your health. This is because progesterone levels naturally reach high levels during pregnancy.
Low progesterone levels can affect both menstruation and fertility. Progesterone helps to promote a suitable environment for a fertilized egg. When progesterone levels are low, it’s harder for a fertilized egg to develop and grow.
Low levels of progesterone can also contribute to certain conditions, including:
If you have low progesterone, there are treatment options available so speak to your GP about them.
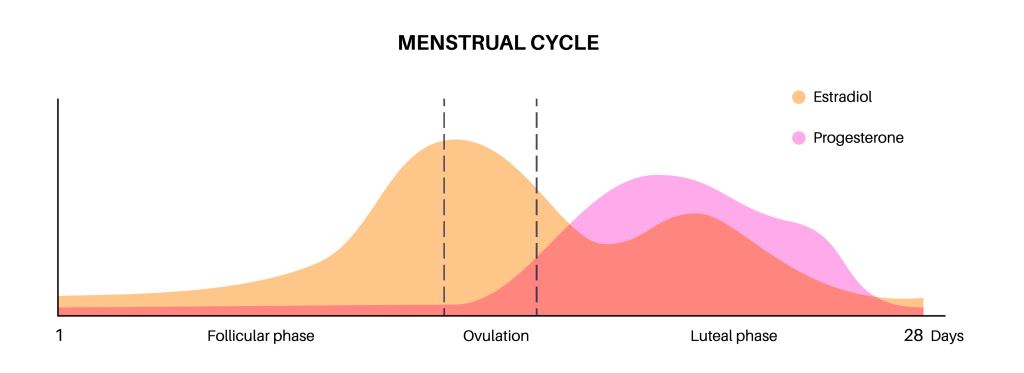
With your LH results, they look for the LH peak to see that you are ovulating. During ovulation, your LH hormone will peak, which releases the egg.
Elevated levels of LH may indicate that the sex organs are not producing sufficient steroid hormones required for reproduction. This often occurs when the ovaries or testes are no longer able to produce estrogen or testosterone due to genetic, autoimmune, surgical, or natural physiological factors.
Low LH levels may indicate a pituitary gland disorder, anorexia, malnutrition, or high levels of stress.
Optimum LH Levels
The optimum luteinizing hormone (LH) levels vary based on factors such as age, sex, and reproductive status. Here’s a general guide for LH levels measured in international units per liter (IU/L):